Life is so uncertain
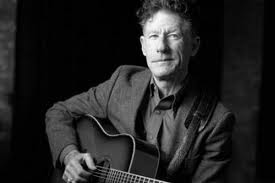
Posted: July 12, 2011 Filed under: breast cancer, tennis | Tags: adjuvant therapy, artificially induced menopause, estrogen, hot flashes, Lupron injection, Lyle Lovett, oncologist visit, oncology, oophorectomy, tamoxifen, tennis, the Wizard of Oz 6 CommentsLyle Lovett said it best:
“Look,
I understand too little too late
I realize there are things you say and do
You can never take back
But what would you be if you didn’t even try
You have to try
So after a lot of thought
I’d like to reconsider
Please
If it’s not too late
Make it a cheeseburger.”
I don’t eat cheeseburgers, or any burgers, but I love Lyle Lovett, and his clever and playful lyrics have been running through my head all day as I contemplated my latest visit to my cutie-pie oncologist. Last time I saw him, we discussed whether I need yet another surgery, to remove my ovaries. See, those little suckers pump out estrogen, and estrogen happens to be fuel for the type I cancer I had. So the theory is this: cut off the fuel, starve the cancer and ensure it has nothing with which to reconvene. Since I wasn’t physically well enough to undergo the oophorectomy because of the post-mastectomy infection, we put that surgery on hold, but in the meantime I began getting a shot of Lupron once every 3 months. Lupron essentially does the same thing as removing the ovaries, which is to shut off the supply of estrogen.
I thought the plan was set: continue the Lupron shots until I was deemed well enough to undergo the oophorectomy, which would likely be in the fall of this year. Get the kids back to school, recover from the August 17th reconstruction revision, and get rid of the ovaries. I like having a plan. I like sticking with a plan. I’m not a fan of changing the plan.
Today, Dr Cutie Pie said he didn’t think I needed to keep getting the Lupron. I’ve been getting the injections for nearly a year now, so even though I was scheduled to get one today and was planning on getting one today, he thought I was done. The plan had changed.
Granted, I had complained to him about the major side-effects of Lupron: hot flashes and sweating like a pig in heat. It’s summertime in Houston. Not just regular old hot-as-Hell summertime in Houston, either, but record heat and record drought summertime. I can tell you with 100 percent certainty that hot flashes and Houston summertime are a wretched combination.
Do I think the hot flashes and sweating like a pig in heat are sound enough reasons to discontinue the current path of hormonal suppression? No. I haven’t murdered anyone (yet). Dr CP said there’s really not that much difference between hormonal suppression from Tamoxifen alone and suppression supplemented even further with Lupron. A year of Lupron injections seemed to be enough, in his opinion. The daily Tamoxifen will go on, though.
Disclaimer: I did not beg, whine, or persuade him to make that decision. Not like I did last summer with Dr S when trying to sway him to release me from yet another hospitalization or disconnect me from the dreaded wound vacuum, Sucky. I did not employ any such tactic with Dr CP today. He came up with the idea to cease & desist all on his own.
He also said maybe that oophorectomy isn’t necessary, either. While I’m completely in favor of eschewing yet another surgery, my gut instinct tells me to rip those ovaries out (gently, though, and with lots & lots of morphine).
Life is so uncertain. What’s the right choice? How does one make such a decision? Stop the Lupron or not? Pursue the oophorectomy or count my blessings that I won’t need another surgery? Where’s the Great and Powerful Oz to tell me what to do?
That’s the problem with cancer. One of the many problems. Big-ass decisions need to be made; life-and-death decisions. And while there’s research aplenty and resources available, there’s no clear answer. I like clear answers. And unchanged plans. Neither of which prevails in one’s “cancer journey.”
Nonetheless, we moseyed along through the rest of the check-up with the usual and quite popular assertions from Dr CP that my cancer is not coming back. I like that part. He says this at every visit, and I really like hearing it. He told me that my reconstructed chest looks fantastic, and I really like hearing that (even though I think he’s shining me on, because there is definitely some tweaking and fine-tuning that needs to be done). I still like that he says it, though, even if he’s shining me on.
We chitty-chatted about his new baby, my tennis game, and other pleasantries. He said he’s started playing tennis and is thinking about taking some lessons. When he told me he plays once a week, I told him he’ll never get better that way; it’s not often enough. He got all puffed up and said it’s enough for him because there’s such a thing as talent.
Oh. Well.
In the immortal words of Steve Martin, “Well, excuuuuuuuuuuuuse me!”
He even strutted down the hallway a bit, then turned to say something about how he’ll be ready in about 6 months to kick my butt on the tennis court. I said, maybe in about 60 years.
How on Earth do I manage to find such cocky doctors?????
We parted ways, him to daydream about beating me in tennis while I headed to the infusion room to get my port flushed. For the last time. Ever.
Yipee! That makes me very, very happy. I’ll get my port removed next month, when Dr S does my reconstruction revision. Can’t wait to bid adieu to that little guy (the port, not Dr S).
But while in the infusion room, I started to second-guess the decision to stop taking the Lupron shots. It didn’t feel right to me. The instant-gratification-girl inside me said, “Hell, yes, let’s forego the shot — that sucker hurts and leaves me bruised for weeks.” But the more-measured-approach-taking girl inside me said something doesn’t seem right with this decision. What’s the harm in continuing the Lupron therapy (besides the obvious, 20-gauge needle harm, that is, and the hot flashes and sweating like a pig in heat harm)?
Dr CP walked by a few minutes later, as I was discussing the pro’s and con’s with my patient advocate extraordinaire, Amy Hoover, and we grabbed him to say I’m not sure about the Lupron decision. He listened intently as we reviewed the pro’s and con’s and said there’s no harm in getting the shot. So I got the shot. Still not sure if it’s the right choice. No idea if it’s the right decision. My gut says yes, and my gut usually is right. However, the fact that it took 3–count ’em–3 tries to get the shot makes me wonder. The needle went in, but the Lupron wouldn’t go. Ow! 3 needle sticks with a 20-gauge needle could easily make a girl question her decision to question her decision. But, as Lyle Lovett says, “Life is so uncertain.”
Oncology report
Posted: April 13, 2011 Filed under: breast cancer | Tags: 20 gauge needle, Arimidex, breast cancer, cancer battle, femara, Jorge Darcourt, Lupron, menopause, oncologist, oncology consultants houston, tamoxifen 8 CommentsMy latest visit to Dr Darcourt was uneventful, which is my favorite kind of doctor visit. Despite the fact that I have to get stuck for blood work and step on the scale every time I go see him, I still like going. As much as you can like going to an oncology visit.
In the beginning of this “cancer journey,” it freaked me out to say “my” and “oncologist” in the same sentence. Not something one usually wishes for, to say the least. But if I have to have an oncologist, my guy is pretty great. Not just because he’s young and Peruvian, either. Although that doesn’t hurt.
Since you’re probably going to google him now, I’ll make it easy on you: 
There ya go.
Just a disclaimer: he was the third oncologist I consulted, and didn’t choose him based on the fact that he’s young and Peruvian. Not just.
Ok, so the appointment was uneventful, and he said the words I love to hear: “I have no reason to think your cancer will come back.” Music to my ears. We talked about Tamoxifen, the chemo pill I take every day and will stay on for 5 years, and the artificially-induced menopause brought on by it and the Lupron shot I get every three months for hormone suppression. In a nutshell, since my cancer was fed by estrogen, it’s easy to control it by depriving it of estrogen. It means I go through menopause a bit early, but that’s a small trade-off for ensuring the cancer doesn’t come back.
The trick is to determine if I’m really in menopause or if once we stop the Lupron shots, we also stop the ‘pause. This is important because it affects the chemo pill I take. Tamoxifen is for pre-menopausal women, i.e., if you weren’t in menopause at the time of diagnosis, you take it. If you’re post-menopausal, you take a different drug, mainly Femara or Arimidex. Either way, I will be on one of these drugs for 5 years. I’m ok with that, because I’m pretty reliable at remembering to take it every day, and it’s another weapon in my arsenal against my cancer.
And taking a pill every day is much easier than getting that Lupron shot. Even though Ionly get it once every 3 months, it’s dreadful. The needle is really big: 20 gauge.
The 20 gauge needle is what is used for port access. It has to be big enough in diameter to not only pierce the skin and the membrane of the port, but also allow for blood to be drawn back out through it.
That’s a big needle.
If you don’t like needles, like me, you may get a little squirmy right about now. That’s ok. Don’t worry if your palms start to sweat, if your heart races, and you feel a little nauseated. All normal reactions to seeing a wonking big needle. But if I have to see it, so do you. I’m good at sharing.
The drug itself is very thick, and has to be warmed before being injected. You know it’s going to hurt. Because it’s thick, it takes several seconds to push the drug through the needle into the body. So the pain lasts. Then once the drug is in, it burns. On the skin and inside. I literally can feel the drug trailing into my body. And yet, I do it willingly. Because I want to starve any cancer cells that may be entertaining thoughts of reforming. I don’t want any uprisings on my watch.
I may take that shot willingly, but I still complain about it. I get it in my left arm, and the bruise from the previous shot, 3 months ago, is always still visible. For several weeks, I will have a hard little knot at the injection site. My arm will be sore for the rest of the day after I get the shot, but then life goes on and it’s business as usual, for the next 3 months.
But yesterday, I made a BIG mistake when getting the shot. I glanced over my shoulder as the nurse was getting ready to inject it. I saw that big-ass needle, glinting in the florescent lights, looking as menacing as an inaninate object can.
Oh, I wish I hadn’t seen that. Somehow the visual reality makes it so much worse. I had to grit my teeth and concentrate on not yelling.
I usually console myself with a beer or a glass of wine on shot days. But yesterday, I was trying to dry out from our Napa trip, so I tried to refrain. I didn’t get very far, and ended up with a Pinot Noir in my glass. But now I’m back to drying out, because I was reading one of my favorite blogs today, and misread one of the lines. It describes waking up and “waiting for the new day to open like a spring margarita.” Oh, wait–it’s
“spring magnolia.” Oops. Guess I’d better get on the wagon, sore arm and all.
A cast of characters, minus one
Posted: February 12, 2011 Filed under: breast cancer, drugs | Tags: Antibiotics, cancer recurrence, morning sickness, pill organizer, pinkwashing, prescription drugs, probiotic, steak, tamoxifen, vegetarian, Walgreens 7 Comments I’ve had this snazzy little grouping of prescription drugs on my kitchen counter for months now. Yes, the lids are pink, because my Walgreens had them for the pinkwashing that comes every October for Breast Cancer Awareness Month. Cute, huh?
I’ve had this snazzy little grouping of prescription drugs on my kitchen counter for months now. Yes, the lids are pink, because my Walgreens had them for the pinkwashing that comes every October for Breast Cancer Awareness Month. Cute, huh?
These are the drugs I take every day, like a little old lady. My old standbys. The usual cast of characters.
There are the two big stars sharing top billing, Bactrim and Minocycline. My darling antibiotics that course throughout my body twice a day, every day to kick some mycobacterium butt. I would be lost without them. Or perhaps I would lose the all-day morning sickness feeling without them, but that’s just wishful thinking. Maybe I’d be dead without them, who knows? There was a time when I was almost sure I was dying from them, but I got over that.
Next we have the Florastor, the one thing that besides coffee that keeps me upright every day. I’m forever indebted to Susan Christopherson for turning me onto this probiotic that helps restore peace and order in one’s digestive system after said system has been under attack by the slash & burn tactics of an antibiotic regime. There have been a few times over the last 6 months of living under this regime in which I’ve either forgotten or willingly neglected the Florastor, and I paid dearly for that mistake. It’s not a prescription, but is kept behind the pharmacy counter for some reason. I don’t have to show my driver’s license to buy it, though, so I guess you can’t make meth out of it.
There’s the Ferrex iron supplement, since I’m a bit anemic and because I need uber-healthy blood vessels to harvest during reconstruction. Because I don’t eat any meat, I need a little help getting my iron; I get some from all the dark, leafy greens I eat, but not as much as my carnivorous friends ingest. My sweet, Peruvian oncologist can’t for the life of himself understand why someone would willingly forego meat. He shakes his head and looks at me a little funny every time it comes up, and he tends to bring it up every time he sees me. I’m done expecting him to compliment me on my plant-based, cancer-fighting diet. It didn’t help much, anyway, so I guess everyone is free to go on ahead and eat a big-ass, nasty, extra-rare steak. Might as well add some fries, or a loaded baked potato. You can see how far the healthy eating thing got me. Harumph.
Then there’s Tamoxifen, my daily cancer-battling bad-ass. It makes sure that there’s no estrogen flowing to feed any remaining cancer cells. While the side effects are troublesome (early menopause, hot flashes, leg cramps, decreased fluid in the joints, to name a few), I like the idea of starving those bastards. Tamoxifen is my first line of defense against recurrence. It makes me feel like I’m doing something every day to keep this beast from re-entering my life. It’s a daily pill that I’ll take for 5 years, then reassess to determine if I should stay on it or switch to another, similar drug.
And today I stopped taking it.
Yikes.
That scares me. More than a little bit. But since Tamoxifen can promote blood clots, it’s counterindicated with surgery. So I stop taking it for 3 weeks and hope that nothing goes haywire with my bloodflow. No clots, no bloodletting, no drama. That sure would be nice for a change.
Although I’m subtracting one prescription from my snazzy little grouping, I still feel like a little old lady whose life revolves around her meds. Ya know the old wisecrack issued when someone asks what time it is, and someone else smarts off, “Why? Ya gotta take a pill?” In my case, the answer is yes, smart ass, more than one pill. So zip it and get me a big glass of water so I can choke these guys down. While my life may seem to revolve around my meds, I refuse–I mean, dig in my heels and refuse–to get a plastic pill organizer. I’m all about accessories, but not that. 
PTSD
Posted: January 21, 2011 Filed under: breast cancer, cancer fatigue, drugs, infection | Tags: breast cancer, Greece, infection, mastectomy, politicians, PTSD, recovery, soldiers, stress, tamoxifen, war 14 CommentsWhile brushing my teeth and inspecting the bevy of brown spots on my face (thanks, crazy hormones), I noticed something that made my heart pound, my stomach drop, and my blood run cold. 
Not to be overly dramatic here, but I was scared. Only for a second, but really and truly scared.
I saw a small dark spot on my jammies top, right near my personal “ground zero” or also known as my right chest wall, site and host of the Mycobacterium Olympics 2010.
My first, terrifying thought was that fluid had leaked from my skin at the site and soaked a spot on my shirt.
Not a good thought.
Turns out it was a small piece of fuzz from a red blanket, but it was in just the right location and was just enough darker than the pink jammie top to look like a wet spot.
It’s been 5 months since my last hospitalization for this wretched infection, yet it still has the power to scare the tar out of me and render me speechless, breathless & frantic for a moment at any given time. There has been (knock wood) absolutely no sign of said infection for those 5 glorious months, but it still freaks me out.
I’ve joked before about having PTSD — post-traumatic stress disorder. Now I’m thinking it’s no joke. Then I see this article, from the Telegraph online. Kismet? You betcha.
The article starts with a catchy lead (y’all know I’m a sucker for a good lead): “The debilitating disorder is often characterised by agitation, anxiety, depression, nightmares, flashbacks, and mood swings. It is more often associated with soldiers returning from battlefields who have been shell-shocked by their experiences.” 
Ok, I admit when I read it, I thought “flashbacks” meant “hot flashes” for some reason. Perhaps because I was suffering from one (hot flash, not flashback) at the moment I read that sentence, and my brain went a little wonky from it.
But here’s the important part: a new study (I also love new studies) has found that women diagnosed with breast cancer have an effect similar to PTSD. Researchers site the effect of diagnosis combined with all the unknowns (surgery? chemo? recurrence? etc) equaling a good chance of developing PTSD. They studied 331 women in a Greek hospital and found that 45 percent showed signs of PTSD. What they did not disclose, however, is how they came up with 331 as their sample size. Inquiring minds would like to know. That seems like an odd number to me, no pun intended. The findings were presented at the Impakt Breast Cancer Conference in Brussels. Now not only do I wonder about the 331 women, but also who in their right mind would spell the name of their conference incorrectly? Impakt? Really? Or is that how “Impact” is spelled in Brussels? Why doesn’t the article tell me these things???
Last year there was a similar study done on the possibility of PTSD in heart attack victims. Seems 1 in 6 heart attackers (16 percent of those studied) suffered from PTSD, while some 18 percent of them exhibited symptoms.
Those kinds of statistics confuse me. Does it mean that 16 percent of the total group studied had full-blown PTSD, while another 18 percent of the same group just had some symptoms? Regardless of the answer to that question, it’s interesting (to me, anyway) that the percentage of breast cancer patients suffering PTSD was so much higher than the percentage of heart attackers who suffered.
Anyhoo…
I’m not a researcher and am not involved in any groundbreaking studies, but I’d guess it’s not just breast cancer that renders its victims full of PTSD. What’s really scary is that women still show signs of PTSD even if their “cancer journey” is complete, with successful treatment and remission of the dreaded disease.
Uh oh. So it’s not enough to accept the diagnosis, endure the surgeries and/or treatments, decide on reconstruction, and monitor our health ad nauseum. We also have to slay the disease, but live with the resulting monkey on our back.
Suck.
They also found that women still suffered PTSD and had a poorer quality of life three years after diagnosis and treatment.
Double suck.
I’m imagining fast-forwarding to 2013, when let’s assume for the sake of this argument my infection is a thing of the past and I’m cruising through life with new girls. Euphemistically speaking; I’m not ditching all my friends and finding new ones. I like ’em all too much to ditch ’em.
Let’s imagine that my “cancer journey” is complete in 2013, except I still take my daily Tamoxifen and see my oncologist every 3 months and get body scans quarterly. I am, for the most part, done. But I’m still going to have PTSD? And a crappier quality of life?
The researchers, from the Panteion University of Athens, warn that doctors should watch out for the signs of the condition when they are treating patients with breast cancer. Those Greek people are smart, gorgeous, and all-around awesome, and everyone on Earth would be wise to listen to and emulate them.
They warn: “Knowing that breast cancer patients are susceptible to PTSD, it might be necessary for the field of medicine to create a plan in assisting cancer patients that takes into account the entire spectrum of a patient’s experience with the illness.”
Emma Pennery, from the British charity Breast Cancer Care, said: “The principle that women, and men, will have an ongoing risk of anxiety and depression following a diagnosis of breast cancer is well known, and there is a range of national guidance in the UK which covers the role of health care professionals in providing ongoing emotional support to patients. ”
I’m curious about that “range of national guidance” and wonder if it will make it across the pond. I certainly haven’t gotten any national guidance in all this. That said, if some form of it came my way, I’d probably scoff at the bloated, partisan jibber-jabber as something dressed up to look valuable but in reality is just an oily politician’s idea of pandering to me and those in my shoes.
But that’s probably just the PTSD talking.
Dear Santa,
Posted: December 22, 2010 Filed under: breast cancer, cancer fatigue, drugs, food, infection, kids | Tags: Bactrim, baseball, Biaxin, bloodwork, bone scan, BRAC, breast cancer, cancer diagnosis, Cefapime, champagne, Christmas, Christmas list, Cipro, collection agency, CT scan, dogs, ER positive, flat chest, genomic testing, good girl, health insurance, HER2 negative, home health, hospital, Houston, infection, infectious disease, injections, IV antibiotics, kids, L-Dex, lymph nodes, mastectomy, minocycline, MRI, PET scan, plastic surgery, post-mastectomy, PR positive, Santa, survivor, tamoxifen, Vancomycin, wound care, wound vac, x-ray, Zyvox 4 Comments I’ve been a pretty good girl this year. I’ve smiled at fussy babies in checkout lines at HEB. I did my time at the grade-school class parties (not my scene, to say the least). I called the collection agency back — yes, I really did — when they left me a message saying I owed money on a past-due hospital bill that my insurance company says has been paid. I donated nearly-new clothes & home goods to charities multiple times. I helped out with the school fundraiser, even though I really, really, didn’t want to. I’ve said please and thank you and bring my own bags. I was a big girl and good sport about all the trips and baseball games I missed this past summer.
I’ve been a pretty good girl this year. I’ve smiled at fussy babies in checkout lines at HEB. I did my time at the grade-school class parties (not my scene, to say the least). I called the collection agency back — yes, I really did — when they left me a message saying I owed money on a past-due hospital bill that my insurance company says has been paid. I donated nearly-new clothes & home goods to charities multiple times. I helped out with the school fundraiser, even though I really, really, didn’t want to. I’ve said please and thank you and bring my own bags. I was a big girl and good sport about all the trips and baseball games I missed this past summer.
And while we’re on the topic of this past summer, dear Santa, do ya remember all the hell I went through? It all started on April 27, 2010, when I was diagnosed with breast cancer. Talk about an “aha” moment. The timeline quickly unfolded like this: the rest of April and first part of May were consumed with tests, tests, and more tests: BRAC analysis, CT scans, x-rays, PET scan, bone scans and MRI. In case that’s not enough acronyms for ya, there was also the L-Dex and then the genomic typing of ER/PR positive and HER2 negative. More injections and blood draws than my poor left arm’s veins could keep up with (literally; there’s a permanent knot in the big vein). Countless appointments with the breast surgeon (Dr Dempsey, who is on the “nice” list) and plastic surgeon (Dr S, who may be on the naughty list), and 3 different oncologists.
Meanwhile, there was research to be done and crushing decisions to be made as I prepared for surgery. The phrase “life and death” took on a whole new meaning, sweet Santa. There’s a strange juxtaposition between packing school lunches and signing field trip permission slips while also filling out my medical directive and living will. I learned pretty fast how to act normal when everything around me had been turned upside down. I think, dear Santa, I also did a pretty good job of adjusting and adapting to the new normal. I think, fat man, I’m still doing a damn fine job of that. One quick look at my profile tells you that there most definitely is a new normal around here.
Santa baby, I was a good girl after the double mastectomy and the lymph node removal that left me battle-scarred and weary. I was an especially good girl in the face of the plethora of prescription drugs I could have used & abused. I was a diligent girl when it came to choosing green drink over Diet Coke, all-natural hormone-free yogurt over Blue Bell.
Santa, I was a brave and good girl when the nasty infection set up shop in my still-raw chest wall. I endured the 103-degree fevers, 22 days in the hospital, multiple tissue excisions and untold poking & prodding without much complaint. I missed the comforts of home, my dogs & my kids more than words can say, but I only cried twice. And even then, it was when no one else was around to see.
We don’t even need to recount the 18 days during which I was attached to the wound vac 24-7. I would really like, dear Santa, to permanently erase that memory from my grey matter, por favor. But I would like to remind you that I was a trouper during the home health days, and all those hours that were consumed with wound care and the administration of IV antibiotics. And while I’m at it, can I get a little shout-out for not killing Dr S, even though he probably deserved it?
Oh Santa, I do crave some credit for all the antibiotics I’ve endured — and continue to endure. From the Vancomycin to Cefapim, from the Cipro to the Zyvox, from the Biaxin to the Bactrim and Minocycline. Those last two will be part of my daily routine for a few months yet, but I’m already looking forward to the day in which I don’t have them on my kitchen counter anymore.
So Santa, how about we make a deal? I’ll set out all the milk & cookies you want in exchange for one little thing. All I want for Christmas is to have it easy for awhile.
A word about menopause
Posted: October 11, 2010 Filed under: menopause | Tags: age spots, breast cancer, cancer battle, ER postivie, estrogen, hormone suppression, hospital, hot flash, Lupron, meno, ovaries, Scrabble, SERM, surgery, tamoxifen, weight gain, world domination 10 CommentsIf you’re a guy, you might not want to read this because it’s, well, about menopause. If you’re a gal who’s not yet experienced the joys of menopause, you might not want to read this because it will scare you. A lot. If you’re brave enough to venture forth, don’t say I didn’t warn you.
Because my cancer was fed by estrogen, after we got rid of the cancer we also had to remove its fuel source, to discourage it from coming back. Hence the stoppage of estrogen. The most direct way to stop the estrogen is to remove one’s ovaries in a lovely procedure called oovectomy (which would also be a seriously high-scoring Scrabble word). If you’re still fighting a wily infection, like me, being cut open in a hospital of all places is a pretty risky move. Especially since the hospital seems the most likely culprit in the age-old question of “How the Hell Do You Even Get an Infection Like That?” While it’s unlikely that my infection would travel from the chest wall to the nether-regions, that’s a chance I don’t want to take, and frankly the idea of another hospital stay gives me the vapors.
Since I’m not ready for the oovectomy, I get the next-best option of hormone suppression, which is a shot of Lupron every 3 months, and a daily dose of Tamoxifen, which is a SERM (selective estrogen receptor modulator) drug. The latter half of that acronym makes me think of something coming out of the Johnson Space Center instead of a prescription bottle from Walgreens, and talk about some great Scrabble words. Build one of those on a triple word spot and you’re damn close to world domination.
So I’m going along in my cancer journey, minding my own business, doing all the things I’m supposed to do, no matter how unpleasant, and yes it’s really good news that the cancer is gone and the infection is on its last legs, too, but do I really have to deal with menopause, too? That just seems mean. You’re seriously going to tell me that battling both cancer and a nasty infection doesn’t exempt one from the hell of menopause? Mean.
I foolishly thought I’d have another decade before having to face the evil triumvirate of menopause: hot flashes, age spots, and weight gain. Even more foolish was the idea that, compared to cancer, menopause would be easy. Silly me.
Living in Houston, land of eternal summer, during hot-flash season, is a challenge. Come to think of it, neither Houston nor hot flashes have a season, so it’s game on, all the time. Local ladies, if you have any remedies for this please pass them on. I have yet to come across a mobile AC unit. I’d be waiting on the doorstep of Radio Shack to purchase said item and would wear it proudly, if only it existed.
So as I’m mopping my sweaty brow after one particularly potent hot flash, I notice some brown spots on my face. Little specs, bigger than freckles but not as big as liver spots. I tried to pick one off, wipe it away, flick it somewhere, anywhere, to no avail. These babies are staying. There’s a constellation near my left eye, and a nice fat one on the inside corner of my right eye. There’s a trio on my forehead, a few singles lingering on my jawline, and God knows where else that I’ve been too busy fighing cancer to really notice up close. Thank you to all my friends for not pointing them out to me. I know you’ve noticed, but were too charitable to tell me I was growing a connect-the-dot game on my face. And there’s a travel version of this game growing on my hands. I’m aging quite visibly as we speak. Thanks, cancer. You bastard.
While the hot flashes are unpleasant and age spots are depressing, the weight gain is really making me mad. I hope there is a special corner of Hell for whoever came up with the hair-brained idea that women will not only lose their breasts but also face scary treatments, complications and all manner of pain & suffering and then gain weight too? That is one messed up system.